SJD Barcelona Children's Hospital was the first centre to use 3D technology to plan cancer surgery for a paediatric patient. Now the centre has gone one step further by creating the 3D Unit.
Virtual simulation and 3D printing are becoming increasingly widespread in the world of health. Five years ago, SJD Barcelona Children's Hospital became the first centre in the world to use 3D technology to plan cancer surgery for a paediatric patient. Now the centre is going one step further in the implementation of this technology by creating the 3D Unit, which is responsible for channelling and assessing the demands of surgical planning, research, prototyping and simulation with 3D models performed by hospital professionals.
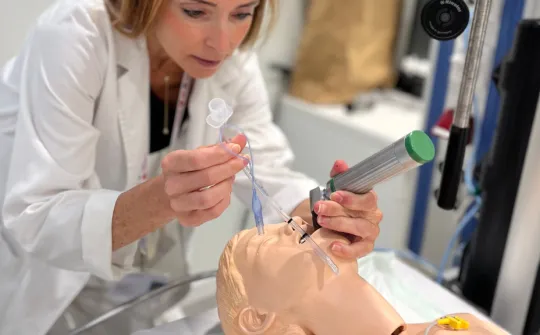
Traditionally, surgeons who had to perform an operation would use scanned images of the diseased organ to plan the intervention. For a number of years, technological advances have enabled the virtual simulation of the anatomical parts involved in the intervention, and if necessary, a life-size, 3D, tailor-made copy printed in a material with a texture similar to the organ in question, allowing them to simulate the intervention as many times as desired before they enter the operating room and providing them with support tools tailored to each patient to guide their steps during an intervention.
The 3D Unit of SJD Barcelona Children's Hospital is organised in a multidisciplinary manner and covers all the centre's departments, channelling the 3D planning requests made by the Hospital's professionals. A committee made up of professionals from various fields, including doctors, radiologists and engineers, receives and assesses the requests made by the professionals.
The centre currently has two 3D printers or additive manufacturing technologies: a PolyJet printer that makes copies with flexible, transparent, soluble and bio-compatible materials, thanks to a donation from Fundación Privada MAR, and a fused deposition modelling (FDM) printer, the SIGMA R19, thanks to a donation from the Fundació CIM of the Universitat Politècnica de Catalunya.
Now, at SJD Barcelona Children's Hospital, virtual simulation and 3D printing are not only used to plan very complex interventions, but also to create personalised prostheses, manufacture surgical tools adapted to the patient and perform practice simulations in teaching activities.
In the field of research, surgeons, radiologists, engineers and researchers from the Hospital are taking part in a European project (ERDF) with a consortium of ten entities renowned in the field of additive manufacturing within the health world, led by the Fundació CIM-UPC. This project aims to improve additive manufacturing systems and bioprinting in the field of critical, reconstructive and regenerative surgery.
Benefits of 3D
According to Arnau Valls, an engineer in the Innovation and Research Department of SJD Barcelona Children's Hospital, the past few years have confirmed the many benefits of 3D planning.
Thanks to virtual simulation and 3D printing, surgeons can plan interventions in an incredibly detailed manner, and this allows them to study and act with precision, and to anticipate and reduce potential surgical complications.
In addition, "3D leads to greater efficiency and efficacy as it helps shorten the length of the intervention and this, once again, impacts the patient, since they receive less anaesthesia. As regards expenses, cost-effectiveness studies are now being published in which the economic benefits are already apparent when interventions for certain diseases are planned in 3D", adds Valls.
An aid in the excision of highly complex tumours
This was the first area to use 3D printing at SJD Barcelona Children's Hospital. The Hospital's Surgery team, with support from Fundació CIM-UPC, was the first in the world to use 3D printing to plan the excision of a highly complex tumour in a paediatric patient. The patient—a five-year-old boy—had a neuroblastoma, an extremely aggressive tumour that forms in the nervous tissue and which proves very difficult to remove due to being surrounded by blood vessels.
Led by surgeon Lucas Krauel, it was decided that a 3D copy of the tumour and organs and vessels involved should be made to carefully analyse the most effective way to approach and remove it without endangering the patient's life, and to rehearse it and again before the intervention, identifying the anatomical relationships of the tumour, vessels and surrounding organs. Eventually, the child underwent surgery and the operation was a success. Since then, 3D has been used in around one hundred of the surgeries performed since 2017 and has been rolled out to other specialities in the Hospital.
3D to correct facial deformities
In the field of maxillofacial and orthognathic surgery, surgeons not only plan the complex and delicate interventions performed to correct facial deformities among children, but even create the surgical tools needed to perform the procedures. Thanks to virtual surgery in 3D, the surgeon Josep Rubio, many days before entering the operating room, studies which of the possible interventions is the most appropriate in each case: in very severe deformities that require distractions, i.e., making a cut to the bone to lengthen it day by day with the help of a device, creating cutting guides using 3D adapted to the physiognomy of the patient to ensure the cut is made in the right place.
3D is also useful in designing the exact measurements of the device that will be fitted on the child to lengthen the bone, since it allows us to make a replica and test it again and again on a 3D copy of the patient's skull. In the past four years, the Maxillofacial Surgery Unit used 3D in the planning and execution of more than 100 interventions.
A highly useful resource for cranial reconstructions
In the field of neurosurgery, 3D is extremely useful for planning detailed interventions before entering the operating room, as well as for creating some of the necessary surgical tools and even tailor-made implants which are thus perfectly adapted to the patient.
The neurosurgery team uses 3D to plan operations for correcting cranial deformities. This is the case, for example, with craniosynostosis, a disease that occurs when the head grows and develops abnormally due to an early closure of the joinings of the different bones that make up the skull.
"This condition creates asymmetry, and to correct it we have to reconstruct the skull by dismantling a part of it. Thanks to 3D, we get a copy of the skull before the intervention which we use to plan what we will do, as well as cutting guides that help to guide us during the surgery and which allow for greater precision", explains Mariana Alamar. The neurosurgeon states that 3D technology is also employed in case of decompressive craniotomies or cranioplasties where there is no bone material from the patient to correct a cranial defect or deformity. In these cases, they create a 3D copy with materials such as porous plastic or titanium. Over the course of 2017, the Neurosurgery Department used 3D in around fifteen operations.
A 3D model for the reconstruction of an ear
Plastic surgeons have also seen multiple possibilities in 3D. Surgeon Francisco Parri, an expert in correcting the microtia or congenital malformation that causes some children to be born with an underdeveloped ear, uses it to create a 3D mirror copy of the healthy ear which will serve as a guide in reconstructing the affected ear. With the 3D copy (until recently they used a flat copy) the surgeons gain a significant degree of precision in the reconstruction of the ear, which is a very difficult operation given the multitude of reliefs and folds presented by this organ.
A tool with many possibilities
Currently, SJD Barcelona Children's Hospital uses 3D printing to plan extremely complex surgical procedures, create cutting guides and surgical tools, design customised prostheses and implants, and perform practical work in the context of teaching and simulation activities.
Most interventions are carried out in the areas of maxillofacial surgery, cancer surgery, neurosurgery, traumatology, cardiology and plastic surgery. Other specialities are starting to test 3D to support their daily clinical practice during complex operations. This is the case, for example, in the SJD Barcelona Children's Hospital Dentistry and Orthodontics Department.